Articles
- Page Path
- HOME > Headache Pain Res > Ahead of print > Article
-
Original Article
Adult-Onset versus Pediatric-Onset Episodic Cluster Headaches: Results from the Korean Cluster Headache Registry -
Pil-Wook Chung1
 , Byung-Su Kim2
, Byung-Su Kim2 , Jeong-Wook Park3
, Jeong-Wook Park3 , Jong-Hee Sohn4
, Jong-Hee Sohn4 , Mi Ji Lee5
, Mi Ji Lee5 , Byung-Kun Kim6
, Byung-Kun Kim6 , Min Kyung Chu7
, Min Kyung Chu7 , Tae-Jin Song8
, Tae-Jin Song8 , Soo-Kyoung Kim9
, Soo-Kyoung Kim9 , Heui-Soo Moon1
, Heui-Soo Moon1 , Kyungmi Oh10
, Kyungmi Oh10 , Soo-Jin Cho11
, Soo-Jin Cho11
-
DOI: https://doi.org/10.62087/hpr.2025.0021
Published online: February 13, 2026
1Department of Neurology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea
2Department of Neurology, Ewha Womans University Mokdong Hospital, Ewha Womans University College of Medicine, Seoul, Republic of Korea
3Department of Neurology, Uijeongbu St. Mary’s Hospital, Uijeongbu, Republic of Korea
4Department of Neurology, Chuncheon Sacred Heart Hospital, Hallym University College of Medicine, Chuncheon, Republic of Korea
5Department of Neurology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Republic of Korea
6Department of Neurology, Nowon Eulji Medical Center, Eulji University, Seoul, Republic of Korea
7Department of Neurology, Severance Hospital, Yonsei University College of Medicine, Seoul, Republic of Korea
8Department of Neurology, Ewha Womans University School of Medicine, Seoul, Republic of Korea
9Department of Neurology, Gyeongsang National University College of Medicine, Jinju, Republic of Korea
10Department of Neurology, Korea University College of Medicine, Seoul, Republic of Korea
11Department of Neurology, Dongtan Sacred Heart Hospital, Hallym University College of Medicine, Hwaseong, Republic of Korea
- Correspondence: Soo-Jin Cho, M.D., Ph.D. Department of Neurology, Dongtan Sacred Heart Hospital, Hallym University College of Medicine, 7 Keunjaebong-gil, Hwaseong 18450, Republic of Korea Tel: +82-31-8086-2310, Fax: +82-31-8086-2317, E-mail: dowonc@naver.com
© 2026 The Korean Headache Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 91 Views
- 2 Download
Abstract
-
Purpose
- This study aimed to compare clinical characteristics between pediatric-onset and adult-onset cluster headache (CH) using data from the Korean Cluster Headache Registry, a nationwide, prospective, multicenter registry.
-
Methods
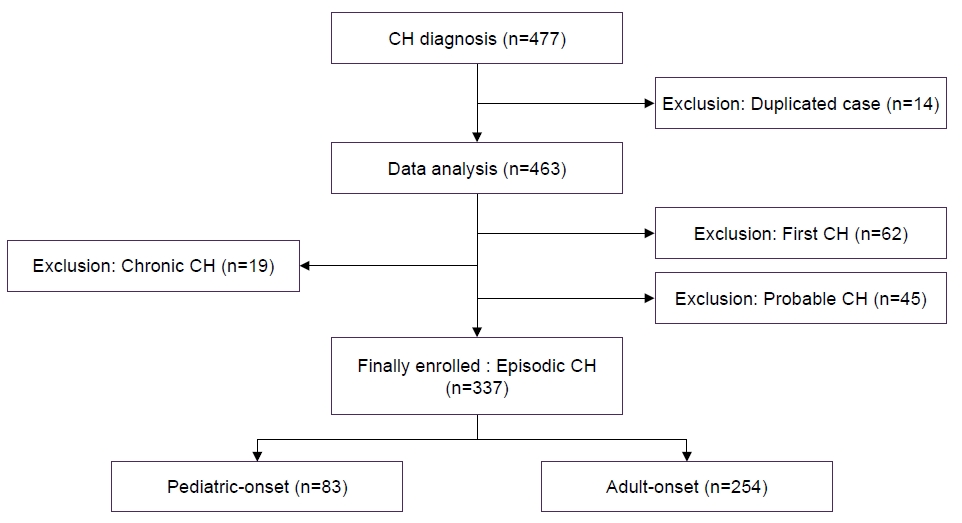
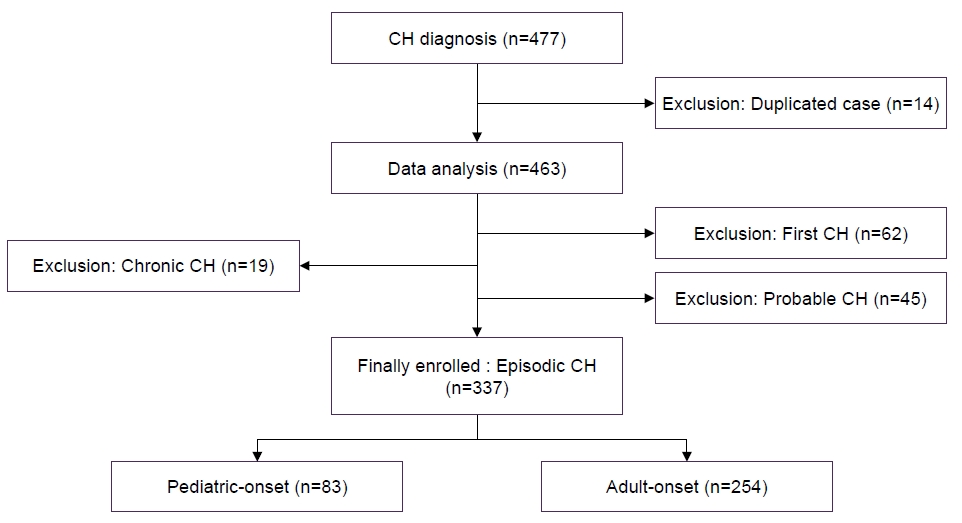
- This cross-sectional observational study analyzed data collected over a 4-year period from a prospective multicenter registry. A total of 337 patients aged ≥19 years with episodic CH were included. Participants were classified as having pediatric-onset CH (onset≤18 years) or adult-onset CH (onset>18 years). Demographic and clinical features, smoking status, and psychiatric comorbidities were compared between groups.
-
Results
- Pediatric-onset CH was reported in 24.6% of patients (n=83). The diagnostic delay was significantly longer in the pediatric-onset group compared with the adult-onset group (10.1 years vs. 6.2 years, p<0.001). Patients with pediatric-onset CH experienced more severe headache attacks (numerical rating scale 9.2 vs. 8.9, p=0.025), although attack duration, frequency, and other clinical features were similar between groups. Smoking exposure was lower in the pediatric-onset group, suggesting potential differences in environmental risk factors. No significant differences were observed in psychiatric comorbidity or headache-related disability.
-
Conclusion
- Pediatric-onset CH is relatively common and shares most clinical features with adult-onset CH, apart from greater attack severity and lower smoking exposure. The longer diagnostic delay in pediatric-onset cases highlights the need for improved awareness and earlier recognition. Further research is warranted to elucidate the underlying pathophysiological mechanisms and long-term outcomes in pediatric-onset CH.
INTRODUCTION
MATERIALS AND METHODS
RESULTS
DISCUSSION
AVAILABILITY OF DATA AND MATERIAL
The data presented in this study are available upon reasonable request from the corresponding author.
AUTHOR CONTRIBUTIONS
Conceptualization: PWC, BSK, SJC; Data curation: PWC, BSK, MJL, BKK, MKC, TJS, SKK, HSM, KO, SJC; Formal analysis: BSK, JWP; Investigation: PWC, JHS, TJS, SJC; Methodology: BSK, HSM, KO; Writing–original draft: PWC, SJC; Writing–review & editing: BSK, JWP, JHS, MJL, BKK, MKC, TJS, SKK, HSM, KO, SJC.
CONFLICT OF INTEREST
Soo-Kyoung Kim is the Deputy Editor of Headache and Pain Research and was not involved in the review process of this article.
Kyungmi Oh is the Associate Editor of Headache and Pain Research and was not involved in the review process of this article.
Soo-Jin Cho is the Editor-in-Chief of Headache and Pain Research and was not involved in the review process of this article.
All authors have no other conflicts of interest to declare.
FUNDING STATEMENT
Not applicable.
ACKNOWLEDGMENTS
Not applicable.
| All patients (n=337) | Pediatric-onset (n=83)† | Adult-onset (n=254)† | p-value | |
|---|---|---|---|---|
| Age (yr) | 37.0±9.8 | 29.6±7.4 | 39.4±9.2 | <0.001 |
| Female sex | 55 (16.3) | 15 (18.1) | 40 (15.8) | 0.619 |
| Current smoker | 151 (44.8) | 23 (27.7) | 128 (50.4) | <0.001 |
| Ever-smoker* | 204 (60.5) | 34 (41.0) | 170 (66.9) | <0.001 |
| Alcohol drinking | 213 (63.2) | 46 (55.4) | 167 (65.7) | 0.09 |
| Coexisting migraine | 44 (13.1) | 10 (12.0) | 34 (13.4) | 0.754 |
| All patients (n=337) | Pediatric-onset (n=83)* | Adult-onset (n=254)* | p-value | |
|---|---|---|---|---|
| Onset age of CH disease (yr) | 26.1±9.9 | 15.7±2.4 | 29.5±9.1 | <0.001 |
| Duration of CH disease (yr) | 10.9±7.2 | 13.9±7.6 | 9.9±6.8 | <0.001 |
| Diagnostic delay (yr) | 7.2±6.9 | 10.1±7.6 | 6.2±6.5 | <0.001 |
| Lifetime bout occurrence (n) | 9.7±10.8 | 14.9±17.6 | 8.0±6.5 | <0.001 |
| Bout frequency (times/yr) | 1.1±2.3 | 1.2±1.4 | 1.1±2.5 | 0.864 |
| All patients (n=337) | Pediatric-onset (n=83)* | Adult-onset (n=254)* | p-value | |
|---|---|---|---|---|
| CH characteristics | ||||
| Attack severity (0–10 NRS) | 9.0±1.2 | 9.2±0.9 | 8.9±1.3 | 0.025 |
| Attack frequency (times/day) | 2.0±2.1 | 1.7±1.3 | 2.1±2.2 | 0.108 |
| Attack duration (min) | 96.2±56.4 | 101.4±47.1 | 94.5±59.1 | 0.33 |
| Duration of bout (wk) | 6.2±5.3 | 6.6±7.1 | 6.1±4.6 | 0.401 |
| Diurnal rhythmicity | 209 (62.0) | 48 (57.8) | 161 (63.4) | 0.138 |
| Seasonal propensity | 182 (54.0) | 45 (54.2) | 137 (53.9) | 0.735 |
| Psychiatric status | ||||
| GAD-7 score | 8.1±6.0 | 7.5±6.1 | 8.3±6.0 | 0.292 |
| PHQ-9 score | 7.8±6.6 | 7.0±6.8 | 8.1±6.5 | 0.174 |
| Suicidal ideation | 79 (23.4) | 22 (26.5) | 57 (22.4) | 0.747 |
| Suicide attempt | 3 (0.9) | 1 (1.2) | 2 (0.8) | 0.757 |
| HIT-6 score | 69.4±7.8 | 70.1±7.0 | 69.1±8.0 | 0.322 |
Values are presented as mean±standard deviation or number (%).
CH, cluster headache; NRS, numerical rating scale; GAD-7, 7-item Generalized Anxiety Disorder scale; PHQ-9, 9-item Patient Health Questionnaire scale; HIT-6, 6-item Headache Impact Test.
*Pediatric-onset was defined as onset age 18 years or less, and adult-onset was defined as onset age more than 18 years.
- 1. Goadsby PJ. Pathophysiology of cluster headache: a trigeminal autonomic cephalgia. Lancet Neurol 2002;1:251-257.ArticlePubMed
- 2. Kim M, Yu JK, Kim YH. Update on cluster headaches: from genetic to novel therapeutic approaches. Headache Pain Res 2024;25:42-53.ArticlePDF
- 3. Rozen TD, Fishman RS. Cluster headache in the United States of America: demographics, clinical characteristics, triggers, suicidality, and personal burden. Headache 2012;52:99-113.ArticlePubMed
- 4. Schor LI, Pearson SM, Shapiro RE, Zhang W, Miao H, Burish MJ. Cluster headache epidemiology including pediatric onset, sex, and ICHD criteria: results from the International Cluster Headache Questionnaire. Headache 2021;61:1511-1520.ArticlePubMedPDF
- 5. Ghosh A, Silva E, Burish MJ. Pediatric-onset trigeminal autonomic cephalalgias: a systematic review and meta-analysis. Cephalalgia 2021;41:1382-1395.ArticlePubMedPDF
- 6. Petersen AS, Lund N, Goadsby PJ, et al. Recent advances in diagnosing, managing, and understanding the pathophysiology of cluster headache. Lancet Neurol 2024;23:712-724.ArticlePubMed
- 7. Taga A, Manzoni GC, Russo M, Paglia MV, Torelli P. Childhood-onset cluster headache: observations from a personal case-series and review of the literature. Headache 2018;58:443-454.ArticlePubMedPDF
- 8. Cho S, Cho SJ, Lee MJ, et al. Clinical characteristics of pre-attack symptoms in cluster headache: a large series of Korean patients. Cephalalgia 2021;41:227-236.ArticlePubMedPDF
- 9. Chung PW, Lee MJ, Park JW, et al. Differences of cluster headache on the basis of sex in the Korean Cluster Headache Registry. Headache 2019;59:1722-1730.ArticlePubMedPDF
- 10. Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia 2013;33:629-808.ArticlePubMedPDF
- 11. Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2013;33:1-211.ArticlePubMedPDF
- 12. Fischera M, Marziniak M, Gralow I, Evers S. The incidence and prevalence of cluster headache: a meta-analysis of population-based studies. Cephalalgia 2008;28:614-618.ArticlePubMedPDF
- 13. Gallai B, Mazzotta G, Floridi F, et al. Cluster headache in childhood and adolescence: one-year prevalence in an out-patient population. J Headache Pain 2003;4:132-137.ArticlePMCPDF
- 14. Zidverc-Trajkovic J, Markovic K, Radojicic A, Podgorac A, Sternic N. Cluster headache: is age of onset important for clinical presentation? Cephalalgia 2014;34:664-670.ArticlePubMedPDF
- 15. Kim BS, Chung PW, Kim BK, et al. Diagnostic delay and its predictors in cluster headache. Front Neurol 2022;13:827734.ArticlePubMedPMC
- 16. Van Obberghen EK, Fabre R, Lanteri-Minet M. Cluster headache diagnostic delay and its predictors: a systematic review with a meta-analysis. J Headache Pain 2025;26:71.PubMedPMC
- 17. van Vliet JA, Eekers PJ, Haan J, Ferrari MD; Dutch RUSSH Study Group. Features involved in the diagnostic delay of cluster headache. J Neurol Neurosurg Psychiatry 2003;74:1123-1125.ArticlePubMedPMC
- 18. Buture A, Ahmed F, Dikomitis L, Boland JW. Systematic literature review on the delays in the diagnosis and misdiagnosis of cluster headache. Neurol Sci 2019;40:25-39.ArticlePubMedPMCPDF
- 19. Maytal J, Lipton RB, Solomon S, Shinnar S. Childhood onset cluster headaches. Headache 1992;32:275-279.ArticlePubMed
- 20. Bastos SNMAN, Barbosa BLF, Silva SF, et al. Cluster headache in children and adolescents: a systematic review of case reports. Dev Med Child Neurol 2021;63:1155-1160.ArticlePubMedPDF
- 21. Levi R, Edman GV, Ekbom K, Waldenlind E. Episodic cluster headache. II: high tobacco and alcohol consumption in males. Headache 1992;32:184-187.ArticlePubMed
- 22. Manzoni GC, Terzano MG, Bono G, Micieli G, Martucci N, Nappi G. Cluster headache: clinical findings in 180 patients. Cephalalgia 1983;3:21-30.ArticlePubMedPDF
- 23. Lund N, Petersen A, Snoer A, Jensen RH, Barloese M. Cluster headache is associated with unhealthy lifestyle and lifestyle-related comorbid diseases: results from the Danish cluster headache survey. Cephalalgia 2019;39:254-263.ArticlePubMedPDF
- 24. Rozen TD. Cluster headache as the result of secondhand cigarette smoke exposure during childhood. Headache 2010;50:130-132.ArticlePubMed
- 25. Rozen TD. Cluster headache clinical phenotypes: tobacco nonexposed (never smoker and no parental secondary smoke exposure as a child) versus tobacco-exposed: results from the United States Cluster Headache Survey. Headache 2018;58:688-699.ArticlePubMedPDF
- 26. Steinberg A, Fourier C, Ran C, Waldenlind E, Sjöstrand C, Belin AC. Cluster headache: clinical pattern and a new severity scale in a Swedish cohort. Cephalalgia 2018;38:1286-1295.ArticlePubMedPDF
- 27. Chung PW, Kim BS, Park JW, et al. Smoking history and clinical features of cluster headache: results from the Korean Cluster Headache Registry. J Clin Neurol 2021;17:229-235.ArticlePubMedPMCPDF
REFERENCES
Figure & Data
References
Citations

 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure
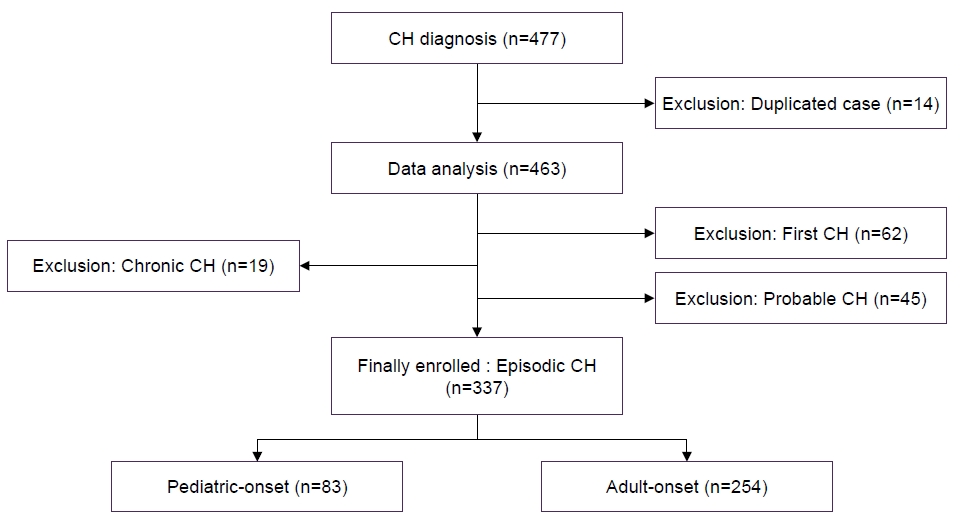
Figure 1.
| All patients (n=337) | Pediatric-onset (n=83) |
Adult-onset (n=254) |
p-value | |
|---|---|---|---|---|
| Age (yr) | 37.0±9.8 | 29.6±7.4 | 39.4±9.2 | <0.001 |
| Female sex | 55 (16.3) | 15 (18.1) | 40 (15.8) | 0.619 |
| Current smoker | 151 (44.8) | 23 (27.7) | 128 (50.4) | <0.001 |
| Ever-smoker |
204 (60.5) | 34 (41.0) | 170 (66.9) | <0.001 |
| Alcohol drinking | 213 (63.2) | 46 (55.4) | 167 (65.7) | 0.09 |
| Coexisting migraine | 44 (13.1) | 10 (12.0) | 34 (13.4) | 0.754 |
| All patients (n=337) | Pediatric-onset (n=83) |
Adult-onset (n=254) |
p-value | |
|---|---|---|---|---|
| Onset age of CH disease (yr) | 26.1±9.9 | 15.7±2.4 | 29.5±9.1 | <0.001 |
| Duration of CH disease (yr) | 10.9±7.2 | 13.9±7.6 | 9.9±6.8 | <0.001 |
| Diagnostic delay (yr) | 7.2±6.9 | 10.1±7.6 | 6.2±6.5 | <0.001 |
| Lifetime bout occurrence (n) | 9.7±10.8 | 14.9±17.6 | 8.0±6.5 | <0.001 |
| Bout frequency (times/yr) | 1.1±2.3 | 1.2±1.4 | 1.1±2.5 | 0.864 |
| All patients (n=337) | Pediatric-onset (n=83) |
Adult-onset (n=254) |
p-value | |
|---|---|---|---|---|
| CH characteristics | ||||
| Attack severity (0–10 NRS) | 9.0±1.2 | 9.2±0.9 | 8.9±1.3 | 0.025 |
| Attack frequency (times/day) | 2.0±2.1 | 1.7±1.3 | 2.1±2.2 | 0.108 |
| Attack duration (min) | 96.2±56.4 | 101.4±47.1 | 94.5±59.1 | 0.33 |
| Duration of bout (wk) | 6.2±5.3 | 6.6±7.1 | 6.1±4.6 | 0.401 |
| Diurnal rhythmicity | 209 (62.0) | 48 (57.8) | 161 (63.4) | 0.138 |
| Seasonal propensity | 182 (54.0) | 45 (54.2) | 137 (53.9) | 0.735 |
| Psychiatric status | ||||
| GAD-7 score | 8.1±6.0 | 7.5±6.1 | 8.3±6.0 | 0.292 |
| PHQ-9 score | 7.8±6.6 | 7.0±6.8 | 8.1±6.5 | 0.174 |
| Suicidal ideation | 79 (23.4) | 22 (26.5) | 57 (22.4) | 0.747 |
| Suicide attempt | 3 (0.9) | 1 (1.2) | 2 (0.8) | 0.757 |
| HIT-6 score | 69.4±7.8 | 70.1±7.0 | 69.1±8.0 | 0.322 |
Values are presented as mean±standard deviation or number (%). *Ever-smokers, current and ex-smokers combined; †Pediatric-onset was defined as onset age 18 years or less, and adult-onset was defined as onset age more than 18 years.
Values are presented as mean±standard deviation. CH, cluster headache. Pediatric-onset was defined as onset age 18 years or less, and adult-onset was defined as onset age more than 18 years.
Values are presented as mean±standard deviation or number (%). CH, cluster headache; NRS, numerical rating scale; GAD-7, 7-item Generalized Anxiety Disorder scale; PHQ-9, 9-item Patient Health Questionnaire scale; HIT-6, 6-item Headache Impact Test. Pediatric-onset was defined as onset age 18 years or less, and adult-onset was defined as onset age more than 18 years.
Table 1.
Table 2.
Table 3.
TOP
 KHS
KHS