Adult-Onset versus Pediatric-Onset Episodic Cluster Headaches: Results from the Korean Cluster Headache Registry
Article information
Abstract
Purpose
This study aimed to compare clinical characteristics between pediatric-onset and adult-onset cluster headache (CH) using data from the Korean Cluster Headache Registry, a nationwide, prospective, multicenter registry.
Methods
This cross-sectional observational study analyzed data collected over a 4-year period from a prospective multicenter registry. A total of 337 patients aged ≥19 years with episodic CH were included. Participants were classified as having pediatric-onset CH (onset≤18 years) or adult-onset CH (onset>18 years). Demographic and clinical features, smoking status, and psychiatric comorbidities were compared between groups.
Results
Pediatric-onset CH was reported in 24.6% of patients (n=83). The diagnostic delay was significantly longer in the pediatric-onset group compared with the adult-onset group (10.1 years vs. 6.2 years, p<0.001). Patients with pediatric-onset CH experienced more severe headache attacks (numerical rating scale 9.2 vs. 8.9, p=0.025), although attack duration, frequency, and other clinical features were similar between groups. Smoking exposure was lower in the pediatric-onset group, suggesting potential differences in environmental risk factors. No significant differences were observed in psychiatric comorbidity or headache-related disability.
Conclusion
Pediatric-onset CH is relatively common and shares most clinical features with adult-onset CH, apart from greater attack severity and lower smoking exposure. The longer diagnostic delay in pediatric-onset cases highlights the need for improved awareness and earlier recognition. Further research is warranted to elucidate the underlying pathophysiological mechanisms and long-term outcomes in pediatric-onset CH.
INTRODUCTION
Cluster headache (CH) is an excruciating form of primary headache disorder that is characterized by recurrent unilateral headache attacks accompanied by ipsilateral autonomic features.1,2 Salient features of CH are its young male predominance, circadian rhythmicity, and trigeminal autonomic features. Although widely varied, CH is prevalent in young adult period with age at onset of CH typically between 20 and 40 years, and suggested to be rare among children. However, recent epidemiologic studies based on self-administered survey showed that 16%–35% of people with CH reported their initial CH attack before the age of 20 years, suggesting pediatric-onset might be underreported.3,4 Clinical features of pediatric-onset CH are similar to adult-onset cases, but diagnostic delay was more frequently reported in pediatric-onset CH, though, there are few studies regarding clinical features of pediatric-onset CH, especially in Asian population.5-7 The aim of this study was to identify different features between pediatric-onset and adult-onset CH using data from the Korean Cluster Headache Registry (KCHR), which prospectively enrolled patients with CH.
MATERIALS AND METHODS
1. Ethics approval and consent to participate
The study protocol and informed consent form were approved by the institutional review board at each hospital (HDT 2016-09-39). Written informed consent was obtained from all participants before they were enrolled in this study. This study was conducted in accordance with the principles of the Declaration of Helsinki.
2. Patients
This study was conducted using data from the KCHR. The KCHR is a prospective, multicenter registry that includes patients with consecutive CH aged ≥19 years across South Korea. Patients were enrolled over 4 years (September 2016 to December 2020) from 15 university hospitals (nine tertiary and six secondary referral centers) and two secondary referral general hospitals. The KCHR protocol has been published previously.8,9 All participants were evaluated by board-certified neurologists in each center and CH was diagnosed using the third edition, beta version of the International Classification of Headache Disorders (ICHD-3b) or the third edition of the ICHD (ICHD-3).10,11 Of the enrolled patients, only patients meeting ICHD-3 criteria for episodic CH were included in this study. Patients were excluded for this analysis if their diagnosis did not meet the ICHD-3 criteria for episodic CH (e.g., chronic CH, probable CH, or first CH) or the patient had missing data.
3. Clinical information
Data obtained and used in the study included the following: demographic factors, present age, age at onset, headache characteristics, seasonal and diurnal rhythmicity, and psychiatric status. Clinical information regarding current headache episodes included the severity, duration, and frequency of headache attacks, and diurnal rhythmicity. The previous history of CH included the onset age of CH, duration of CH disease, total number of cluster bouts, and pattern of seasonal periodicity. The personal history of cigarette smoking was obtained and used to classify patients into ever-smokers and never-smokers. Ever-smoker patients were further classified into current and former smokers.
4. Statistical analysis
Demographics and clinical features were compared between pediatric-onset and adult-onset patients. Pediatric-onset was defined as onset age 18 years or less, and adult-onset was defined as onset age more than 18 years. The two-sample t-test were used to compare the mean values between pediatric-onset and adult-onset cases. The chi-square test or Fisher’s exact test was used to compare categorical variables. Probability values of p<0.05 were considered indicative of statistical significance. All analyses were performed using the Statistical Package for the Social Sciences (version 29.0; IBM Corp.).
RESULTS
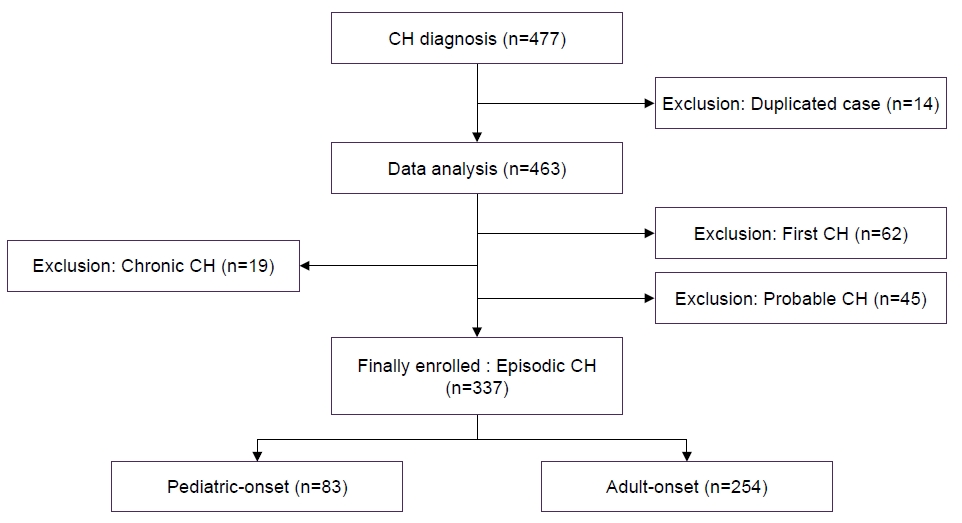
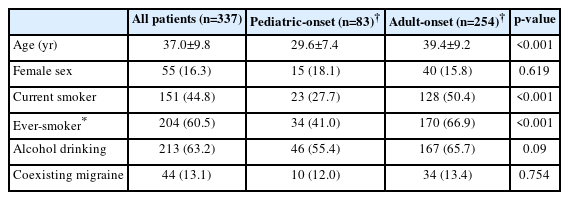
The KCHR is a prospective, multicenter registry that enrolled patients with CH aged ≥19 years. Among the 463 patients identified as having CH in the KCHR, 337 met the criteria for episodic CH according to the ICHD-3. Of the remaining 126 patients, 19 patients were diagnosed with chronic CH, 45 were diagnosed as probable CH, and the remaining 62 presented with the first CH period and neither categorized as episodic nor chronic CH. Therefore, 337 patients with episodic CH were included in this analysis (Figure 1). The age at enrollment was higher in the adult-onset CH group compared to the pediatric-onset CH group (39.4±9.2 years vs. 29.6±7.4 years). In the pediatric-onset CH group, 15 (18.1%) were female, and in the adult-onset group, 40 (15.8%) were female. There was no statistically significant difference in the sex ratio between pediatric- and adult-onset CH (Table 1). A total of 151 patients (44.8%) were current smoker, and 204 patients (60.5%) were ever-smoker (comprising current and ex-smokers). The prevalence of smoking differed significantly between pediatric and adult-onset group. Twenty-three (27.7%) were current smokers in pediatric-onset group and 128 (50.4%) were current smokers in adult-onset group (p<0.001). The proportion of ever-smokers was also lower in the pediatric-onset group than in the adult-onset group (41.0% vs. 66.9%, p<0.001) (Table 1).
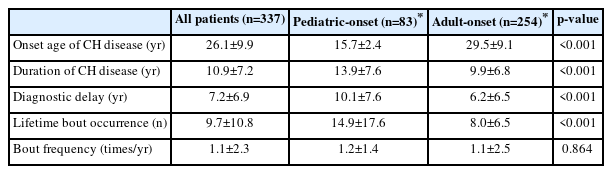
Eighty-three (24.6%) participants reported an age of onset of 18 or younger (pediatric-onset), while 254 reported an age of onset after 19 years old. Disease history was compared between the pediatric-onset and adult-onset patients. The age at onset was 15.7±2.4 years (range, 9–18 years) in pediatric-onset patients and 29.5±9.1 years (range, 19–55 years) in adult-onset group. The time from onset to diagnosis of CH was prolonged in both groups, with pediatric-onset cases experiencing a notably greater delay in diagnosis (10.1±7.6 years [range, 0–31 years] vs. 6.2±6.5 years [range, 0–32 years], p<0.001) (Table 2).
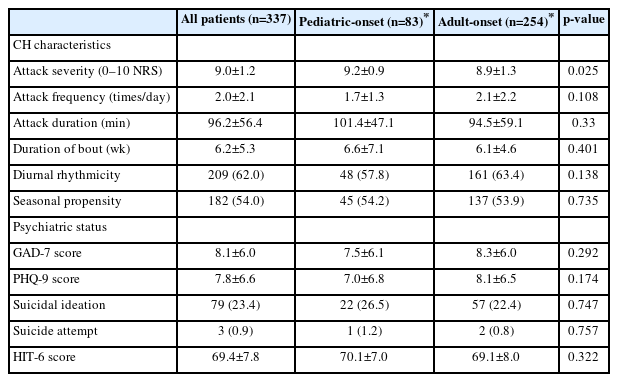
Headache characteristics were compared between pediatric- and adult-onset patients. Headache attack was more severe in pediatric-onset patients based on numerical rating scale (9.2±0.9 vs. 8.9±1.3, p=0.025). However, attack duration and daily attack frequency did not differ between the groups. There were no significant differences in bout frequency (mean number of bouts per year), duration of cluster period, diurnal rhythmicity, and seasonal propensity in both groups (Table 3). Depression scale assessed by 9-item Patient Health Questionnaire scale and anxiety scale based on 7-item Generalized Anxiety Disorder scale did not differ between pediatric and adult-onset CH. Headache-related disabilities, as determined by 6-item Headache Impact Test also did not differ (Table 3).
DISCUSSION
Main findings of present study were as follows: 1. Eighty-three out of 337 patients (24.6%) reported onset of CH in 18 years or younger, indicating that pediatric-onset CH is not uncommon. 2. Diagnostic delay of pediatric-onset CH is more severe than adult-onset CH. 3. Smoking exposure rate is lower than that of adult-onset case (all patients were evaluated in adult age). 4. Clinical features are generally similar to adult-onset CH, except more severe attack in pediatric-onset cases.
CH is a rare primary headache disorder with a prevalence of around 0.1% in general population.12 It is generally known to occur most frequently in young adult males, and studies and reports are rare in pediatric patients. In this study, 24.6% (n=83) of 339 patients who met the criteria of episodic CH reported initial onset of CH during pediatric period (18-year or younger). Previous studies regarding pediatric-onset CH and/or pediatric CH is scarce and mostly based on case series or single clinic observations, therefore, epidemiologic data regarding pediatric CH is still elusive.6,12 An Italian multicenter study reported that out of 6,629 childhood headache patients, 3 were diagnosed with CH, suggesting 1-year prevalence of childhood CH at 0.03%.13 In United States CH survey study, 35% of 1,134 patients reported CH began at 20 years or younger.3 International study using self-administered survey showed pediatric-onset (<18 years old) was found in 27.5% (341/1,583) of participants.4 Both studies have a limitation of questionnaire or survey-based method of CH diagnosis. A previous headache clinic-based study reported that 16% of CH patients experienced early onset (before age of 20).14 In contrast, the present study, which utilized a nationwide prospective registry, found that 24.6% of Korean participants with episodic CH reported an onset of CH at 18 years of age or younger. Although the age criteria of pediatric-onset CH varied among studies, the proportion of pediatric-onset cases in the present study is generally consistent with findings from Western or international research. Taken together, these results suggest that CH frequently begins during pediatric years.
Although clinical features of CH is characteristic and easily recognizable, there is no reliable biomarker available for its diagnosis. Therefore, early diagnosis of CH remains a challenge because many patients with CH experience delayed diagnosis or misdiagnosis.15,16 Given the severe pain associated with CH attacks, such delays or misdiagnoses could have a significant impact on both patients and society as a whole. Our study demonstrated that diagnostic delay was more severe in pediatric-onset patients. Diagnostic delay was 10.1 years in pediatric cases, compared to 6.2 years in adult-onset CH patients. Our result confirms previous studies, which suggested younger age at onset as a factor for diagnostic delay of CH.7,14,17,18 International CH questionnaire study found only 15.2% of participants with pediatric-onset were diagnosed before the age of 18.4 The reasons for more delay in pediatric cases are unclear. Pediatric CH might be more difficult to diagnose because features of migraine are often frequently found in pediatric CH.7 Furthermore, pediatric migraine attack can be as short as 2 hours, and overlap in attack duration between migraine and CH in child could make diagnosis even more difficult.5 Studies have indicated that the duration of CH attacks in children may fall below the lower limit observed in typical CH attacks.7 Pediatric headache specialist are fewer than adult headache specialist, therefore, lack of access to physician might be another reason for diagnostic delay.4
Clinical features of pediatric-onset CH was similar to adult-onset cases in this study, except for slightly more severe headache attack in pediatric-onset CH (9.2±0.9 vs. 8.9±1.3, p=0.025). However, headache feature analysis was based on current CH attacks (all patients enrolled after 19 years old) and we could not identify whether headache features changed from their original headache features in pediatric ages. Clinical and autonomic features of early onset CH were similar to adult-onset CH in other reports.16,19,20 Pediatric-onset patients display the full range of each criterion for CH in a previous systematic review.5 Cranial autonomic features and restlessness occur at a lower rate in pediatric cases, while migraine features such as nausea, photophobia, and phonophobia were found similarly to adult-onset patients.5
Although pathophysiologic associations are unknown, epidemiologic studies have shown that cigarette smoking is closely associated with CH.21-23 Previous study has even suggested that secondary smoke exposure during childhood may be related to the subsequent development of CH.24 Our study found that patients with pediatric-onset CH were less frequently exposed to smoking. Proportion of current smoker and ever-smoker in pediatric-onset cases were lower than those of adult-onset CH in this study. In line with our study, other studies demonstrated that CH not exposed to smoking were more likely to develop CH at a lower age than exposed patients.25,26 Lower smoking exposure in pediatric-onset cases suggests a genetic or biology-based etiology in pediatric-onset CH, while higher smoking rate in adult-onset CH is suggestive of the smoking-related environmental etiology in adult-onset patients.25,27 However, a lower age at CH onset could cause patients to avoid smoking habit, so the influence of smoking before and after the onset of CH needs to be investigated further.27 Nonetheless, the relationship between smoking exposure and CH warrant cautious interpretation. Age, sex, and cultural background could markedly confound the smoking habitus. In particular, the significantly higher mean age in the adult-onset CH group may have provided greater opportunity for smoking exposure in the adult-onset participants in our cohort. Accordingly, until additional validation is conducted, our findings should be considered preliminary and hypothesis-generating.
There are several limitations in the present study. First, the patients included in this study were individuals whose headache onset occurred during childhood or adolescence, but who were evaluated during adulthood. Some clinical features of pediatric CH can only be accurately assessed through direct observation during the pediatric period, and, as a result, recall bias may have affected our findings. Although long-term, prospective studies following CH from childhood into adulthood would provide the most reliable data, conducting such research is challenging due to the rarity of CH and the difficulties associated with its diagnosis in pediatric populations. Second, in this study, we did not investigate the differences of treatment responses between pediatric and adult-onset CH. Third, the participants in this study consisted only of Korean patients referred to a secondary or tertiary hospital, and so the results might not be generalizable to all patients with CH, especially those with milder forms of the disorder or other ethnicity. Lastly, our analysis was limited to patients with episodic CH, excluding those with chronic CH or probable CH. Chronic CH was very rare in our cohort, representing only 4.1% (19/463) of the entire sample. Since episodic CH is the most typical and prevalent form, focusing on strictly defined episodic CH may be more valuable for identifying the characteristics of pediatric-onset CH. Nevertheless, further research is warranted to investigate chronic CH and the long-term changes over time in patients with pediatric-onset CH.
Notes
AVAILABILITY OF DATA AND MATERIAL
The data presented in this study are available upon reasonable request from the corresponding author.
AUTHOR CONTRIBUTIONS
Conceptualization: PWC, BSK, SJC; Data curation: PWC, BSK, MJL, BKK, MKC, TJS, SKK, HSM, KO, SJC; Formal analysis: BSK, JWP; Investigation: PWC, JHS, TJS, SJC; Methodology: BSK, HSM, KO; Writing–original draft: PWC, SJC; Writing–review & editing: BSK, JWP, JHS, MJL, BKK, MKC, TJS, SKK, HSM, KO, SJC.
CONFLICT OF INTEREST
Soo-Kyoung Kim is the Deputy Editor of Headache and Pain Research and was not involved in the review process of this article.
Kyungmi Oh is the Associate Editor of Headache and Pain Research and was not involved in the review process of this article.
Soo-Jin Cho is the Editor-in-Chief of Headache and Pain Research and was not involved in the review process of this article.
All authors have no other conflicts of interest to declare.
FUNDING STATEMENT
Not applicable.
ACKNOWLEDGMENTS
Not applicable.